Research
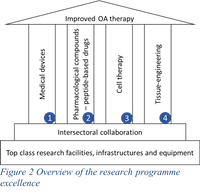
Osteoarthritis (OA) is the most frequently diagnosed joint degenerative disease and the biggest growing chronic disease in the Netherlands. It is anticipated that the OA patient population will double towards 2.2 million patients in 2040 in the Netherlands alone, and towards hundreds of millions worldwide. The number of years during which patients experience pain and disability due to OA is rapidly increasing and one of the underlying causes can be found in the global increase of life expectancy. Despite the growing OA epidemic and major socio-economic impact, the population is facing a staggering lack of disease-modifying therapies that can preserve joint function by preventing cartilage- and joint degeneration and delaying OA progression. This leaves invasive total joint replacement as the only currently available option to treat the consequences of end-stage OA. However, considering the increase in life expectancy, a demanding active life-style and an unexplained growing number of young OA patients, costly and high-risk revision surgery of the primary prosthesis is a growing major problem that we should be solving by delaying the need for total joint replacement by innovations from basic research. The OSTASKILLS project is based on a research programme comprising four major pillars, providing the doctoral candidates training in the clinical development and market introduction of medical devices, pharmaceutical products and advanced therapy medicinal products in the area of joint repair. They are overarching and cross-fertilizing major domains and levels of life science and will feed entrepreneurial training of scientists to translate key basic science findings towards meaningful clinically applicable interventions. These 4 pillars, topic-wise, cover currently promising key approaches to support the preservation of joint function, repair of cartilage defects and prevent OA
Pillar 1 | Medical devices
Lead | Marcel Karperien – Twente University
Other partners | Pieter Emans – Maastricht University
Background Cartilage defects caused by trauma or ageing are an important risk factor for disturbance of joint homeostasis and development of OA.
Translational innovations To address this risk factor and postpone OA development, Twente University has developed a polymeric formulation capable of long-term intra-articular filling cartilage defects of different sizes and shapes, inducing regeneration of the damaged cartilage. Excellent pre-clinical results have been achieved in equine models and the technology is now ready for clinical introduction. Maastricht University is developing a non-degradable polymeric composite (sub-)chondral plug with cartilage-like biophysical properties, to repair focal (osteo)cartilage defects for middle-aged (35-65 yrs.) patients who, due to their calendar age or joint age, are not capable to regenerate their cartilage.
Patient’s opportunities These two medical devices are now ready for clinical implementation and subsequent market introduction. The doctoral candidates will contribute to the development of the required ISO certified quality management systems, the design, implementation and execution of the clinical trial and the development of a medical device dossier suited for submission to the notified body.
Needed to bring innovation forward in 5 years to come Successful clinical and market innovation in medical devices for cartilage repair field depends on the acquisition of a CE mark provided by the notified body. The doctoral candidates will have the opportunity to explore all aspects of building a medical device dossier needed for obtaining such approval.
Benefits for the doctoral candidates Successful innovations in the field of cartilage repair depends on the easiness of the surgical procedure and handling of the medical device, the potential for surgical introduction in a minimally invasive manner, its success in cartilage regeneration and/or replacement and thereby restoring joint homeostasis for low costs. The above described technologies meet these criteria. Both products target specific patient populations and have largely completed preclinical testing. They are now ready for clinical introduction and seek to obtain a CE mark for market introduction. Given the infancy of the trajectory ultimately leading to market introduction in 5 years, at earliest timepoint, from now, provides ample opportunity for the doctoral candidates to experience and familiarize with all aspects needed for building a medical device dossier. We offer training in a basic research laboratory, an academic medical centre as well as in the participating SMEs which intend to bring the technology to the market. This provides a unique opportunity to approach the goal from different perspectives. With the recent introduction of the medical device regulations (MDR) in the EU much uncertainty exists in the approaches that should result in obtaining a CE mark for a medical device. The doctoral candidates will get hands on experience with this new regulation which will make them ideally suited for positioning themselves for a career in a company that plans to certify new medical devices after completion of their training.
Pillar 2 | Pharmacological compounds – peptide-based drugs
Lead | Tim Welting – Maastricht University
Other partners | Marcel Karperien – Twente University, other partners | Wurzburg University
Background Pharmacologically treating (early) OA or conditioning the joint homeostasis after cartilage trauma shall become an important avenue to attenuate the progression of OA-related cartilage-/joint destruction, or prevent initiation of cartilage pathology following cartilage damage, respectively.
Translational innovations Several key growth factors and druggable pathways have been identified in the past decades that are capable of regenerating cartilage and attenuating OA development. However, drug-based treatment of cartilage pathologies comes with critical challenges that are quite unique for the joint: the synovial space is a harsh environment for biologics and treatment of a single joint with biological agents must be applied locally (intra-articular). Due these challenges the targeting of key druggable pathways for cartilage regeneration and OA treatment with biological agents is hampered. Local intra-articular treatment using growth factors is largely incompatible with the synovial space due to their molecular instability. To overcome this important limitation, Maastricht University has a fundamental research program on the discovery and mechanism-of-action of bioactive peptides from key growth factors (such as BMP-7) for cartilage regeneration and OA treatment, to mitigate cell biological processes like cartilage hypertrophy and cartilage formation. Based on this research selected lead peptide compounds are being developed for future clinical application and investigating pharmacokinetics, pharmacodynamics and safety of lead peptide compounds for intra-articular application.
Another clinically promising route to alter joint pathological molecular processes, while circumventing the challenging nature of the joint, is the use of VHHs (variable domain of heavy chain only antibodies). The University of Twente has developed VHHs that can induce tissue regeneration and/or reduce pain. VHHs have various advantages over conventional antibodies. They are small and extremely stable, consist of a single peptide chain and are equally effective in antigen binding and/or neutralization in comparison to conventional antibodies. VHHs are amenable for facile genetic modification optimizing antibody properties and due to their small size, they can be cost effectively produced using bio fermentation processes in yeast for a fraction of the costs of conventional antibodies. Particularly relevant for cartilage repair VHHs can easily penetrate the dense cartilage matrix in contrast to the impaired capacity of conventional antibodies to reach the cartilage embedded chondrocytes. VHHs thus have great potential to translate into an antibody based intra-articular injection therapy to mitigate processes like pain by blocking the NGF/TrkA pathway, inflammation by neutralizing inflammatory cytokines and or activation of cartilage formation by targeting growth factors and/or chondrocytes.
University Hospital of Regensburg (UHREG) has great expertise with patient-derived chondrocytes as well as with and 3D in vitro hypertrophy model for chondrogenically differentiating human Mesenchymal Stem Cells (MSCs). Moreover, human chondrocytes can be isolated (under approved and running ethical grants at UHREG) from cartilage trauma patients as well as early and late state OA patients and thereafter, cultivated in vitro. In collaboration with Maastricht and Twente Universities the effects of bioactive peptides and VHHs will be evaluated on the clinically relevant cell types available in UHREG. Furthermore, the bio-active peptides will be implemented in the in vitro hypertrophy model and evaluated for their ameliorating potential of MSC conversion to hypertrophic chondrocytes.
Patient’s opportunities Peptides and VHHs are novel biologic agents that can potentially be used for the treatment of cartilage pathologies to influence the homeostasis of the joint and or reduce joint pain/inflammation, thereby preventing/modifying OA and reducing OA clinical symptoms.
Needed to bring innovation forward in 5 years to come Successful clinical implementation of above-mentioned biopharmaceutical compounds depends on many success factors. One of them is patient stratification. To obtain more insight into disease heterogeneity on an individual patient level, the doctoral candidate will contribute to implementing cell biological assays for stratifying responder and non-responder cartilage defect- and OA patients. The doctoral candidate will contribute to investigating pharmacokinetics and pharmacodynamics of novel intra-articular drug compounds and will be involved in further developing peptide and VHH technology to be able to clinically validate the technology. This involves steps including the humanization of the VHH technology; peptide/VHH GMP production/purification and GLP tox, and relevant animal experiments including clinical trials in animal patients before proceeding to clinical trials.
Benefits for the doctoral candidates Pharmacologically treating intra-articular pathologies, like cartilage defects and OA, requires out-of-the-box non-classical pharmacological approaches, to acquire enough local compound concentrations and to reach target cells effectively/selectively. In addition, it is becoming increasingly evident that cartilage defect- and OA patients are a heterogeneous group of patients, with subpopulations that ideally need to be stratified for responsiveness-to-therapy. Furthermore, doctoral candidates will learn isolation, cultivation and investigation of clinically relevant patient-derived chondrocytes. In addition, fundamental knowledge on disease stage related chondrocyte phenotypes will be gained. The candidate work will contribute to understanding the patient response to the pharmacological cues as well as optimize the effectiveness of anti-hypertrophy agents. This will improve the potential outcome of clinical trials and, upon clinical implementation, will improve the cost effectiveness of these treatments. Given these basic prerequisites and challenges for future intra-articular treatment strategies, the doctoral candidate will benefit from a multidisciplinary environment in which ample opportunities for training in design of bioassays/compound screening, patient stratification, biotechnology, pharmacokinetics, pharmacodynamics and regulatory requirements for drug development.
Pillar 3 | Cell therapy
Lead | Ivan Martin & Andrea Barbero – University of Basel
Other partners | Twente University – Wurzburg University – Lund University
Background In the past decade it has become clear that cell therapy for preserving joint homeostasis can be highly effective and the paracrine actions of diverse preparations of mesenchymal stems have been demonstrated to attenuate the development of OA. Similar properties have recently ascribed in neuroectodermal derived nasal chondrocytes. Standardization of cell preparations and effective local delivery and retainment/survival of the therapeutic cells poses a hampering issue in this field that must be addressed to safeguard this promising development for patient use soon.
Translational innovations University of Basel has demonstrated that cartilage tissues engineered by adult nasal chondrocytes maintain their cartilaginous properties after being exposed in vitro to a variety of inflammatory factors. Experiments performed in microfluidic devices showed that the secretome of nasal chondrocytes positively influences the inflammatory profile of OA cells. In in vivo models, tissue generated by nasal chondrocytes efficiently integrates into the adjacent native OA tissues, along with survival of the implanted cells. Such properties were observed even once nasal chondrocytes were immediately implanted in vivo after their isolation from the cartilage biopsy. In collaboration with UHREG, crosstalk between the nasal chondrocytes and cartilage trauma and OA chondrocytes will be investigated in vitro to outline paracrine cellular communication and expected benefits of the therapeutic strategy.
Patient’s opportunities nasal chondrocytes isolated using a rapid isolation protocol can be encapsulated in gel and thus used for a single-stage cartilage repair approach.
Needed to bring innovation forward in 5 years to come A phase I clinical trial would be mandatory to assess the safety and feasibility of intraoperative injection of nasal chondrocytes for the treatment of cartilage lesions.
Benefits for the doctoral candidates This pillar will support the training of doctoral candidates on in vitro and ex vivo studies, using chondrocytes, the use of specifically designed bioreactors allowing control over the tissue environment and the use of microfluidics systems platform allowing to investigate in a high-throughput manner cells/tissue responses to bioactive factors. The recruited doctoral candidates will have a unique opportunity to acquire complementary expertise (cell biology, biomaterials science and bioengineering) and to be in contact with different backgrounds and actors of the regenerative medicine field. The doctoral candidates will have the possibility to acquire considerable networking opportunities for their future career. Moreover, the doctoral candidates will have the possibility to get several high-quality peer-reviewed publications that will contribute to increase the quality of their CV.
Pillar 4 | Tissue-engineering
Lead | Martin Stoddart – AO Research Institute Davos
Other partners | Maastricht University – Wurzburg University - Lund University
Background Tissue engineering of cartilage is one of the earliest fields of regenerative medicine that started developing decades ago, and only now we start to understand all critical aspects of the combination of cellular biology, biomaterials and molecular signals, to properly engineer cartilaginous constructs for implantation. Although tissue-engineering approaches for cartilage repair and osteoarthritis have been developed over the past decades, the implementation of these therapies in clinical practice and standard of care has been slow and often limited. True cartilage regeneration rather than the formation of fibro-cartilage tissue remains unsolved and there is still an important need to further improve our understanding and develop improved Tissue engineering approaches. To do so there is a need to improve 1) the cell delivery, survival and action through enhanced biomaterials, 2) define the mechanism of action of the implanted cells (e.g. chondrocytes, stem cells) and control their fate (e.g. avoid hypertrophy), 3) develop more relevant in vitro models for screen of tissue engineering solutions.
Translational innovations Maastricht University is developing an autologous in situ manner to generate subperiosteal cartilage from residing stem cells for treating focal cartilage defects. The AO Research Institute Davos is developing autologous mesenchymal stromal cells tissue engineered solutions. A numerical model is being developed to design 3D printed biomaterial scaffolds for optimal mechanotransduction of embedded stem cells for their differentiation toward a chondrogenic phenotype in absence of growth factors and under mechanical load mimicking knee joint kinematic. A multiaxial mechanical load bioreactor is developed and used to assess effect of mechanical load patterns and optimize tissue-engineering solutions. In order to gain insights into the integration process of engineered cartilage constructs to the surrounding cartilage tissues, UHREG will investigate in collaboration with AO institute the response of clinically relevant cartilage trauma and OA derived chondrocytes to the cartilage analogs engineered in this pillar. Moreover, the biomaterials designed in this pillar will be evaluated in the UHREG established 3D in vitro hypertrophy model with chondrogenic human MSCs.
Patient’s opportunities The understanding gained in studying the effect of compression and shear loads on the chondrogenic differentiation of different sources of stem cells can now be potentially translated by designing better post-operative physiotherapy for improved stimulation and recovery of patients.
Needed to bring innovation forward in 5 years to come Numerical model applied to the design of 3D printed scaffolds for cartilage tissue engineering allowing for more robust response of cells therapy under optimized physiotherapy protocols.
Benefits for the doctoral candidates We aim to make significant advance towards the introduction of regenerative therapies for cartilage repair and treatment of osteoarthritis (OA) into the clinic. Therefore, doctoral candidates that can develop new therapies while keeping clinical and regulatory conditions in mind are needed for developing new solutions and their future exploitation. By offering a comprehensive training program that encompasses an extensive range of interdisciplinary skills and addresses the recognized gap in knowledge and clinical translation, we will train a new generation of scientists that can be the mediator between fundamental and basic science on one hand and clinical uptake and application on the other hand.