Exploring Osteoarthritis Through In Vivo Models
Julius-Maximilians-University (JMU) of Wuerzburg
Viviana Reyes
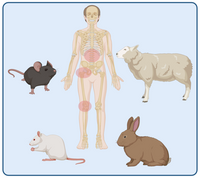
“Furry Allies in Osteoarthritis Research: Understanding Osteoarthritis through Animal Models ”
Osteoarthritis (OA) is a complex degenerative joint disease characterized by progressive cartilage loss, inflammation, and structural changes in the affected joints. Understanding the pathophysiology of OA and developing effective therapies rely heavily on preclinical research, often using animal models to mimic human disease conditions. In vivo models play a crucial role in OA research, providing insights into disease mechanisms, evaluating potential treatments, and advancing translational medicine. In this post, we explore into the significance of in vivo models in OA research and highlight some common models used in the field.
Importance of In Vivo Models in OA Research
1. Mimicking Human Disease: In vivo models allow researchers to replicate key features of human OA, such as cartilage degradation, synovial inflammation, subchondral bone changes, and joint stiffness. By studying these models, researchers can better understand disease progression and identify potential therapeutic targets.
2. Assessing Treatment Efficacy: In vivo models are instrumental in evaluating the efficacy of novel therapies for OA. Whether testing pharmacological agents, biological interventions, or regenerative techniques, these models provide a platform to assess treatment outcomes, safety profiles, and long-term effects on joint health.
3. Investigating Disease Mechanisms: By using in vivo models, researchers can investigate the underlying molecular and cellular mechanisms driving OA pathogenesis. This includes studying the role of inflammatory mediators, matrix-degrading enzymes, oxidative stress, genetic factors, and biomechanical influences in joint tissue homeostasis and breakdown.
4. Translational Relevance: Successful translation of experimental findings to clinical practice requires robust preclinical models that recapitulate human OA pathology. In vivo models bridge the gap between basic research discoveries and clinical applications, facilitating the development of more targeted and effective OA therapies.
Commonly Used In Vivo Models in OA Research
1. Surgical Induction Models:
- Destabilization of the Medial Meniscus (DMM): This model involves surgical destabilization of the medial meniscus in rodents, leading to altered joint biomechanics and progressive cartilage degeneration reminiscent of human OA.
- Anterior Cruciate Ligament Transection (ACLT): ACLT surgery in animals disrupts knee joint stability, resulting in cartilage erosion, subchondral bone changes, and osteophyte formation over time.
2. Naturally occurring OA Models: Certain strains naturally develop spontaneous OA, without the need of any surgical intervention. The OA manifestation is variable, which makes it more like the OA observed in human cases.
3. Chemical Induction Models:
- Monosodium Iodoacetate (MIA): Injection of MIA into joint spaces induces rapid and reproducible joint degeneration by inhibiting glycolysis in chondrocytes, leading to cartilage damage and pain-like behaviors in animals.
- Collagenase-Induced OA (CIOA): Intra-articular injection of collagenase enzymes initiates cartilage breakdown and joint inflammation, mimicking certain aspects of OA pathology.
3. Genetically Modified Models:
- Mice with Specific Gene Knockouts or Mutations: Genetically engineered mice lacking key genes involved in cartilage maintenance, inflammation, or matrix remodeling can elucidate molecular pathways contributing to OA development and progression.
4. Obesity-Associated Models:
- Diet-Induced Obesity Models: High-fat diet regimens in animals lead to obesity, metabolic dysfunction, and joint loading alterations, mimicking obesity-related OA seen in humans.
- Leptin or Leptin Receptor Deficient Models: Leptin plays a role in energy metabolism and inflammation; therefore, leptin-deficient models can highlight the impact of metabolic factors on OA pathophysiology.
5. Traumatic Injury Models:
- Joint Impact or Fracture Models: Inducing joint trauma or fractures in animals can trigger post-traumatic OA changes, including cartilage degeneration, synovitis, and subchondral bone remodeling, similar to human post-traumatic OA.
Challenges and Considerations in In Vivo OA Research
1. Species Variability: While animal models provide valuable insights, species differences in joint anatomy, biomechanics, and immune responses necessitate careful interpretation and validation of findings in human tissues.
2. Disease Heterogeneity: OA is a heterogeneous disease with variable phenotypes and underlying mechanisms among patients. In vivo models may not fully capture this complexity, highlighting the need for diverse models and personalized medicine approaches.
3. Ethical and Regulatory Considerations: Researchers must adhere to ethical guidelines and regulatory standards when using animals in research, ensuring humane treatment, proper care, and transparent reporting of methodologies and outcomes.
4. Translational Validation: Findings from animal studies must be validated in human clinical trials to confirm therapeutic efficacy, safety, and relevance to patient outcomes, emphasizing the importance of interdisciplinary collaborations and translational research efforts.
Future Directions and Innovations
1. Advanced Imaging Techniques: Utilizing high-resolution imaging modalities such as micro-CT, MRI, and ultrasound enables non-invasive longitudinal monitoring of joint changes in live animals, enhancing OA research and treatment assessments.
2. Biomechanical and Biomarker Analyses: Integrating biomechanical assessments and biomarker analyses in in vivo models provides comprehensive insights into joint function, tissue biomechanics, and molecular signatures associated with OA progression and treatment responses.
3. Cell-Based Therapies and Tissue Engineering: Advancements in cell-based therapies, tissue engineering, and biomaterials hold promise for developing regenerative approaches targeting damaged cartilage, synovium, and subchondral bone in OA joints, revolutionizing future treatment strategies.
In conclusion, in vivo models are indispensable tools in osteoarthritis research, offering valuable insights into disease mechanisms, treatment efficacy, and translational relevance. By leveraging diverse animal models, innovative technologies, and interdisciplinary collaborations, researchers aim to unravel the complexities of OA and develop transformative therapies for improved patient outcomes and joint health.
References: